Oorspronkelijk artikel
Focal ischemia on [13N]NH3-PET/CT after stent placement: two cases
- 18-02-2025
- Leestijd: 3 minuten
Remco JJ Knol, MD, PhD; Friso M van der Zant, MD, PhD; Maurits Wondergem MD, PhD; Sergiy V. Lazarenko, PhD
Department of Nuclear Medicine, Noordwest Ziekenhuisgroep, Alkmaar, The Netherlands
Inleiding
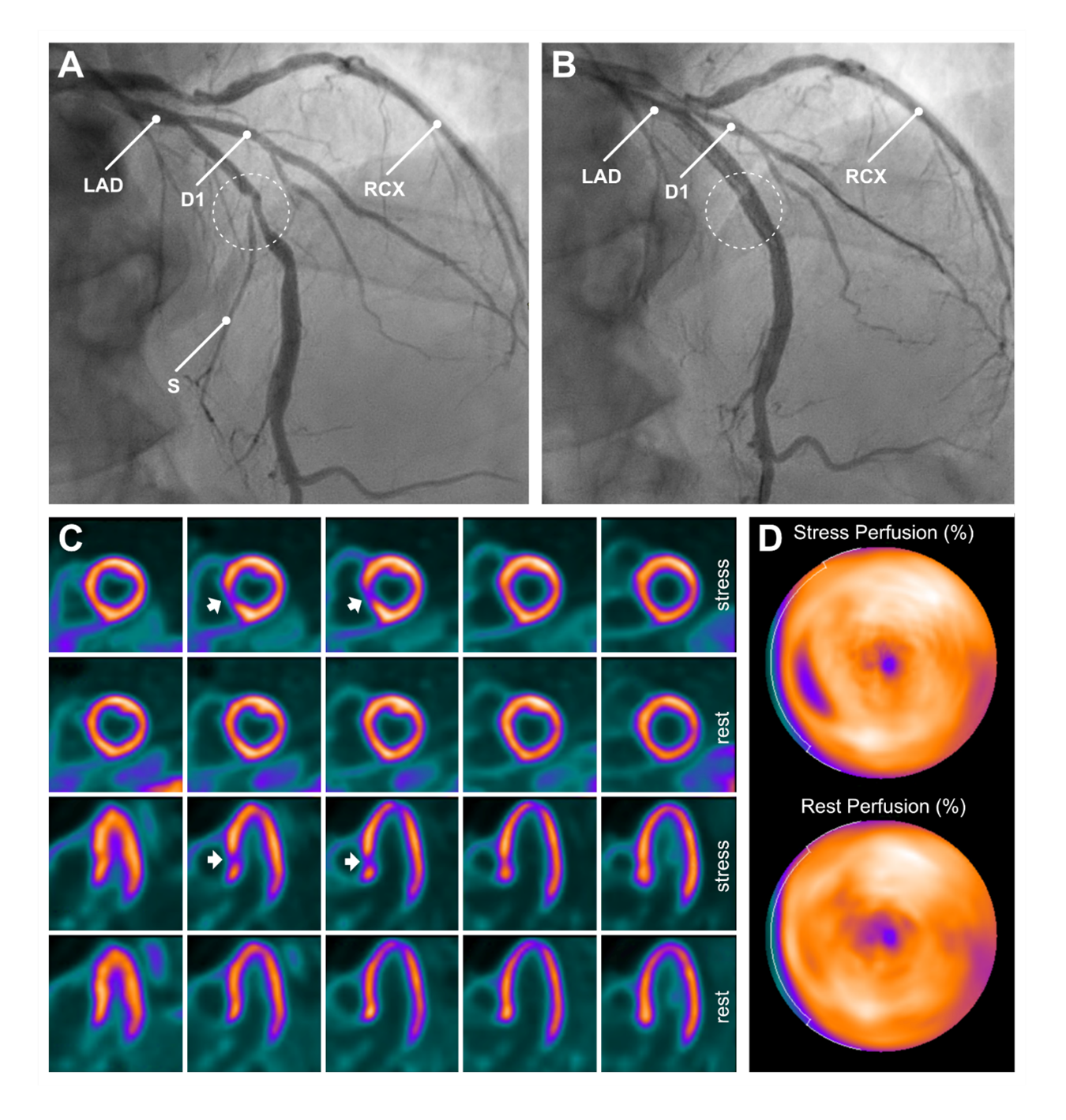
Case 1: A 69-year-old man with a low cardiovascular risk profile was admitted to the cardiology department due to progressive angina pectoris and unstable angina, despite ongoing anti-anginal medication. In the months preceding admission, the patient had been evaluated for exertional chest pain, and a recent calcium scoring CT had revealed substantial three-vessel calcifications. At the time of admission, cardiac enzyme levels were within normal limits. Coronary angiography (CAG) demonstrated severe three-vessel disease, with the right coronary artery (RCA) identified as the likely culprit lesion. The case was reviewed by the multidisciplinary heart team, and the patient was scheduled for percutaneous coronary intervention (PCI) of the mid-RCA (not shown), a bifurcation lesion in the mid left anterior descending (LAD) (Panel A, dashed circle), and ramus circumflexus (RCX), with placement of three drug-eluting stents (DES) in total. Following stent placement, the LAD angiogram showed loss of visualisation of a septal branch (S) (Panel B, dashed circle).
The occurrence of bifurcation lesions is around 15-20% (1,2). With PCI of these lesions, there is a 5-9% risk of side-branch occlusions (SBOs) (1-5). Independent risk factors for the occurrence of SBOs include the bifurcation angle (smaller angle has a higher risk), diameter of the side branch, the magnitude of side branch and main vessel stenosis and plaque burden, the main vessel lesion length, the preprocedural flow of the side branch, irregular plaque and PCI in the context of an acute coronary syndrome (4-6).
In the years after stent placement, the patient continued to experience anginal symptoms during strenuous physical activity. A [13N]NH3-PET/CT scan was performed to evaluate for significant ischemia. This scan revealed a small area of focal ischemia on the short and horizontal long axes in the septal myocardium (Panel C (arrows) and D), likely corresponding to the occluded side branch observed post-stenting. The PET/CT scan showed neither evidence of significant ischemia nor infarction. Because of low positron range in tissue (mean 1.5 mm), [13N]NH3-PET/CT has excellent spatial resolution and is therefore suitable for detection of perfusion abnormalities in patients after revascularisation, including small perfusion defects resulting from SBOs (7,8). Exercise tolerance of the patient was good, symptoms were manageable, and the cardiac condition was stable. Consequently, optimal medicinal therapy (OMT) was deemed the appropriate course of action.
Case 2: A 71-year-old female visited the cardiologist because of exertional chest complaints. She had risk factors for cardiovascular disease, including hypertension, overweight and a positive family history of coronary artery disease. Treadmill exercise study provoked recognisable complaints with slight ST-depression on the electrocardiogram. CAG was performed and showed three-vessel disease. After review of the multidisciplinary heart team, a multivessel PCI was performed with stenting of the mid-LAD, the distal RCA (Panel A, dashed circle) and, one year later, of the proximal RCX.
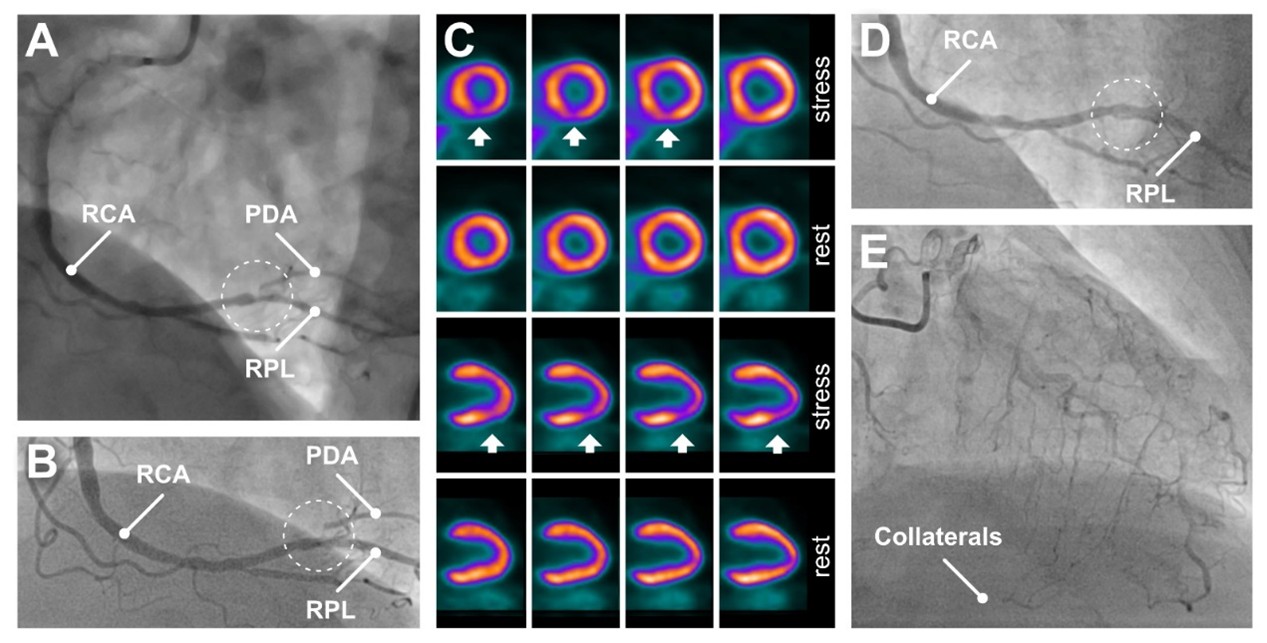
CAG after stenting at the transition of the RCA to the right posterolateral (RPL) branch shows a stent in the RCA but still a stenosis at the origo of posterior descending artery (PDA) (Panel B, dashed circle).
Four years after the initial presentation, the patient presented with dyspnoea on exertion and radiating pain to the left arm. Evaluation for ischemia was carried out by means of [13N]NH3-myocardial perfusion PET/CT. During adenosine stress, dyspnoea without chest pain, was experienced. The electrocardiogram showed non-specific ST-segment depression (1 mm) in leads II, III, aVF and V4 to V6.
Short axis and vertical long axis views (Panel C) show a small reversible defect in the inferior left ventricular wall (arrows) matching occlusion of the PDA. It remains unclear whether the ischemia is caused by progression of the pre-existing ostium stenosis, stent jailing or both. The patient was started on long-acting nitrates and a diuretic, which provided some relief of symptoms.
Two years after [13N]NH3-PET/CT, the patient presented again with progressive complaints of angina pectoris. CAG shows occlusion of the PDA (Panel D, dashed circle) and collateral filling from the LAD (Panel E). After discussion in the multidisciplinary heart team, it was concluded that the occluded branch was too small for intervention. The patient was treated pharmacologically by switching her calcium antagonist and diuretics, but she remained symptomatic.
Case 1 demonstrates acute SBO, which in general could be caused by carina shifting, plaque shifting, plaque embolisation, thrombus formation, spasm, or dissection as a direct result of stent placement (2,6,7,9). Several side branch protection and rescue techniques have been proposed to prevent SBO during PCI or to address it once detected, yielding mixed clinical outcomes (6). Case 2 shows an example of late SBO, which might develop due to progression of a pre-existent plaque or formation of a new plaque within or around the stented segment. The consequences of SBO are variable and dependent on the used technique. Restoration of flow can occur spontaneously (5-14%) or after intervention (5-55%), but a considerable part (31-90%) remains occluded (4,5). At present, the exact clinical relevance of SBOs is not fully understood. Some studies show an increased risk of major adverse cardiac events, especially cardiac death and myocardial infarction (3,5), while other studies showed no differences in clinical outcome (4,9).
Referenties
- Zhang D, Yin D, Song C, et al. A randomised comparison of Conventional versus Intentional straTegy in patients with high Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion: rationale and design of the CIT-RESOLVE trial. BMJ Open. 2017;7(6):e016044
- Stankovic G, Darremont O, Ferenc M, et al. European Bifurcation Club. Percutaneous coronary intervention for bifurcation lesions: 2008 consensus document from the fourth meeting of the European Bifurcation Club. EuroIntervention. 2009;5(1):39-49
- Muramatsu T, Onuma Y, García-García HM, et al. Incidence and short-term clinical outcomes of small side branch occlusion after implantation of an everolimus-eluting bioresorbable vascular scaffold: an interim report of 435 patients in the ABSORB-EXTEND single-arm trial in comparison with an everolimus-eluting metallic stent in the SPIRIT first and II trials. JACC Cardiovasc Interv. 2013;6(3):247-57
- Zhang D, Xu B, Yin D, et al. Predictors and Periprocedural Myocardial Injury Rate of Small Side Branches Occlusion in Coronary Bifurcation Intervention. Medicine (Baltimore). 2015;94(25):e992
- Hahn JY, Chun WJ, Kim JH, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol. 2013;62(18):1654-9
- Li D, Dai H, Gao C, et al. Review of Techniques for Protecting Side Branch from Occlusion during Provisional Stenting in Coronary Bifurcation Lesions. Rev Cardiovasc Med. 2023;24(11):323
- Kan H, Knol RJ, Lazarenko SV, Wondergem M, van der Zant FM. Occurrence of typical perfusion defects attributed to jailed or occluded side branch after ramus descendens anterior stenting in a patient cohort referred for 13NH3 myocardial PET/CT. Nucl Med Commun. 2016;37(5):480-6
- Driessen RS, Raijmakers PG, Stuijfzand WJ, Knaapen P. Myocardial perfusion imaging with PET. Int J Cardiovasc Imaging. 2017;33:1021-31
- Iñiguez A, Macaya C, Alfonso F, et al. Early angiographic changes of side branches arising from a Palmaz-Schatz stented coronary segment: results and clinical implications. J Am Coll Cardiol. 1994; 23:911-5
Samenvatting
This case report focusses on two symptomatic patients with focal ischemia on [13N]NH3-PET/CT, occurring either directly or in the years after stenting of coronary artery stenoses. These cases demonstrate bifurcation stenoses of the LAD/septal branch, and the distal RCA/PDA respectively, with remaining ischemia after stenting and subsequent occlusion of the jailed side branch.